- Open-Access Publishing
- Quality and Potential Expertise
- Flexible Online Submission
- Affordable Publication Charges
- Expertise Editorial Board Members
- 3 Week Fast-track Peer Review
- Global Visibility of Published Articles
Persistent Left Superior Vena Cava with Unusual Drainage
Sanjana Shah1*, Abhisheik Prashar2, Victar Hsieh2, George Youssef2, Walid Matar3, Queenie Lo2
1St. George Hospital, Gray Street, Kogarah, NSW 2217, Australia
2Department of Cardiology, St. George Hospital, Gray Street, Kogarah, NSW 2217, Australia
3Department of Neurology, St. George Hospital, Gray Street, Kogarah, NSW 2217, Australia
*Corresponding Author: Sanjana Shah, St. George Hospital, Gray Street, Kogarah, NSW 2217, Australia, E-mail: sanjanashah.91@gmail.com
Received date: July 11, 2021; Accepted date: August 04, 2021; Published date: August 11, 2021
Citation: Shah S, Prashar A, Hsieh V, Youssef G, Matar W, et al. (2021) Persistent Left Superior Vena Cava with Unusual Drainage. J Card Cardi Sur. 1:06.
Copyright: © 2021 Shah S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Persistent left superior vena cava; Cerebrovascular accident; Transesophageal echocardiography; Venous to systemic shunt; Paradoxical embolism
Abstract
We present the case of an unusual drainage pattern involving a Persistent Left Superior Vena Cava (PLSVC) in a patient who presented with a bi-hemispheric stroke for investigation. This case report highlights a less common drainage pattern of PLSVC into the left atrium, which has implications for a number of clinical scenarios including investigation for possible source of systemic embolic phenomena and procedures requiring central venous catheterisation. We also illustrate the utility of echocardiography and other non-invasive imaging modalities in the diagnosis of this anomaly.
Introduction
Ischemic cerebrovascular accidents (CVA) are more common in patients with congenital heart defects as compared to the general population [1]. The role of paradoxical embolization in the causation of CVAs is also well established. Thrombo-emboli are shunted from its origin in the venous circulation to the systemic circulation via an intra-cardiac or pulmonary shunt [2]. Persistent Left Superior Vena Cava (PLSVC), a thoracic venous anomaly, is one such cause of paradoxical emboli when it drains into the left heart [3]. This case report describes an unusual presentation of stroke attributed to an uncommon drainage pattern of PLSVC into the Left Atrium (LA) through the left superior pulmonary vein.
Case presentation
A 64-year-old man presented to the emergency department with sudden onset of expressive aphasia and confusion. There was no associated limb weakness, paresthesia, facial droop or visual disturbance. His past medical history was significant for type 2 diabetes mellitus and hypertension with no previous cerebrovascular accidents (CVAs). His cardiovascular physical examination was normal with no audible murmurs on auscultation and no evidence of deep venous thrombosis in his upper and lower limbs. His electrocardiogram was notable for sinus bradycardia. A Computed Tomography Angiogram (CTA) of the head and neck was performed which showed trace intimal plaques at the origin of both common carotid arteries without any significant stenosis along with complete occlusion of the left vertebral artery with retrograde flow distal to the occlusion.
A Magnetic Resonance Imaging (MRI) scan of the brain was performed which demonstrated infarcts in both cerebral hemispheres (Figure 1). Cardiac telemetry for one week during his hospital stay did not demonstrate atrial fibrillation or other emboligenic arrythmias. Venous ultrasounds of bilateral upper limbs did not show any evidence of venous thrombosis. An acquired thrombophilia screen performed was negative. The patient underwent a transthoracic echocardiogram (TTE) followed by a transesophageal echocardiogram (TEE) which showed normal cardiac chamber sizes and normal coronary sinus appearance (Figure 2). There was no evidence of inter-atrial defects, patent ductus arteriosus or valvular abnormalities. No thrombus was visualized in the left atrium (LA) or its appendage. There was no evidence of atherosclerotic disease in the thoracic aorta.
A bubble study was performed using peripheral intravenous cannulas in both arms. A bolus of agitated gelofusine administered via a peripheral intravenous cannula in the left arm showed immediate contrast opacification of the LA before the right atrium (RA), indicative of a venous to systemic shunt. When another bolus of agitated gelofusine was injected via a peripheral intravenous cannula in the right arm, normal contrast filling was demonstrated in the RA first (Figure 3). A cardiac Computed Tomography (CT) scan was performed to investigate the anatomy of the thoracic venous system. It confirmed the presence of a PLSVC draining into the left superior pulmonary vein and subsequently into the LA (Figure 4). The risks and benefits of surgical closure were discussed with the patient, who declined surgery. A non-vitamin K antagonist oral anticoagulant (NOAC), apixaban, was commenced as secondary prevention of further embolic events. The patient was discharged home after making a full neurological recovery. He was followed up in the cardiology clinic and remained well with no further strokes or bleeding complications at 12 months after the initial presentation.
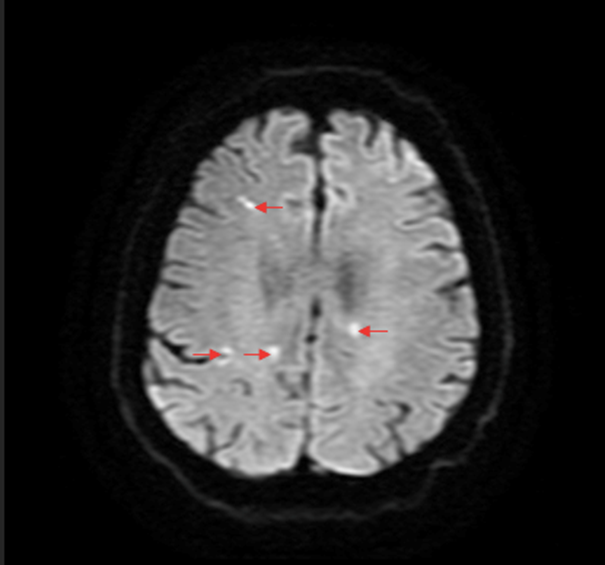
Figure 1: Magnetic resonance imaging of the brain-diffusion weighted image: Multiple hyperintense signals (arrows) in both cerebral hemispheres.
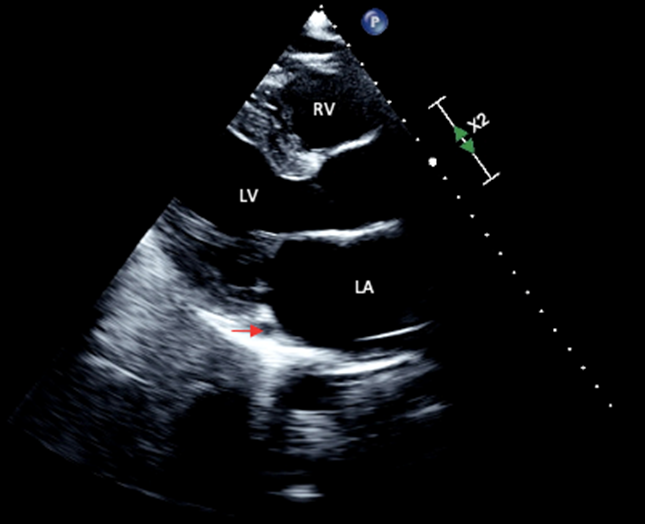
Figure 2: Transthoracic echocardiogram-parasternal long axis view: Normal Left Ventricular (LV) size and systolic function and a non-dilated coronary sinus (arrow). Abbreviations: RV=Right Ventricle; LA=Left Atrium.
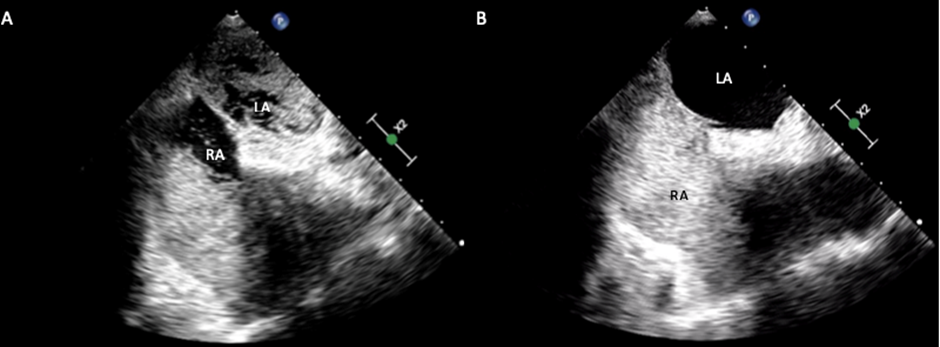
Figure 3: Transoesophageal echocardiogram-mid-oesophageal view. 3A: Bubbles entering into the Left Atrium (LA) before the Right Atrium (RA) from a left sided intravenous cannula. 3B: Bubbles entering into the RA before the LA from a right sided intravenous cannula.
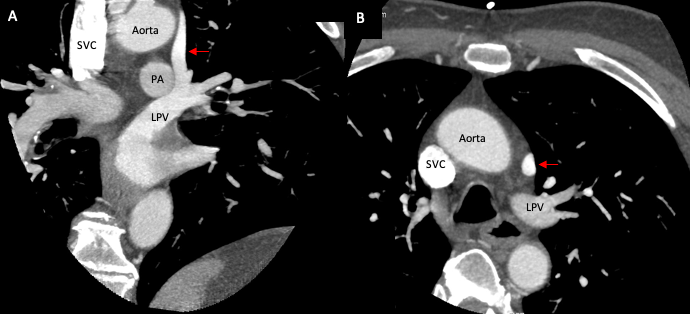
Figure 4: Cardiac computed tomography-oblique view: Persistent left superior vena cava (arrow) draining into the Left Pulmonary Vein (LPV). Abbreviations: SVC=Superior Vena Cava; PA=Pulmonary Artery.
Discussion
A PLSVC is an uncommon congenital anomaly of the thoracic venous system with a prevalence of 0.3% to 0.5% in the general population [3-5]. When present, it originates at the junction of the left internal jugular vein and subclavian vein. It travels downwards, anterior and to the left of the main pulmonary artery and enters the atrio-ventricular groove posterior to the left atrial appendage [4,6]. It drains into the RA through the coronary sinus in 80-90% of cases. However, in 8-10% of cases, it drains into the LA either directly or indirectly through an unroofed coronary sinus or a pulmonary vein causing a venous to systemic shunt, such as in our case [3,4,7]. Other sites of drainage include inferior vena cava and hepatic vein [7,8].
It is important to consider the embryology of the formation of the thoracic venous system in order to understand the anatomical variations in patients with PLSVC. In the fetus, two pairs of cardinal veins, -the anterior and posterior, drain the cephalic and caudal portion respectively. They in turn drain into the heart via the left and right common cardinal veins which are connected through the innominate vein. The internal jugular vein is formed by the cephalic portion of the anterior cardinal veins. The caudal portion of the right anterior cardinal vein along with a part of the right common cardinal vein form the right sided superior vena cava. Normally, the caudal portion of the left anterior cardinal vein involutes to form the ligament of Marshall, the failure of this process results in the formation of the PLSVC [6,7,9].
A PLSVC draining into the RA is usually asymptomatic. In most cases, it is diagnosed incidentally on cardiovascular imaging or during procedures that require central venous catheterization along with insertion of pacemaker and defibrillator leads [3,10,11]. These procedures can be made challenging in patients with undiagnosed PLSVC with complications such as hypotension, cardiac dysrhythmia, angina, cardiac tamponade and even cardiac arrest [5,12-16].
A venous-to-systemic shunt is formed when the PLSVC drains directly into the LA. This can disseminate thrombi and even air, introduced via central and peripheral catheters, into the systemic circulation causing end-organ infarcts including a CVA [6,17]. Recto et al. reported a case demonstrating a temporal correlation between the injection of saline from a left sided cannula and the development of stroke-like symptoms in a patient with PLSVC draining into the LA via the pulmonary vein [18]. There have been other studies implicating PLSVC in the causation of intra-cerebral abscess [17,19]. It is also associated with an increased risk of mild arterial desaturation, cyanosis and heart failure [2,3,6]. In our case, the bi-hemispheric nature of the infarct involving multiple vascular territories was suggestive of a proximal source of embolization. Also, there was no arrhythmia identified on seven days of cardiac telemetry. Hence, the PLSVC causing paradoxical embolization was considered as the most likely etiology. Minor trauma to the left upper extremity was postulated to cause clot formation and paradoxical embolization via the PLSVC, although no obvious venous thrombi were detected on an ultrasound of the upper limbs [6].
An echocardiogram-TTE or TEE, is a non-invasive and effective tool that can be used to identify this condition. Coronary sinus defects can be identified through echocardiography. About 75-83% cases of unroofed coronary sinus are associated with PLSVC [20]. A bubble study should be performed using peripheral intravenous cannulas in both arms. This can illustrate the presence of any abnormal thoracic venous drainage or cardiac shunts [20]. It is worthwhile to note that the left upper limb veins preferentially drain into the PLSVC when it is present [18,19]. Hence, in the absence of a connection between the two superior vena cavae, the shunt will only be demonstrated when the left upper limb is used to deliver the bubble contrast injection. Park et al also demonstrated this correlation in a recent case report where a patient presenting with multiple strokes was mislabeled as cryptogenic when routine stroke workup failed to identify a PLSVC. On index presentation, an echocardiogram with bubble contrast study was only performed through a right upper limb peripheral cannula. As in our case, a PLSVC causing paradoxical embolism was only identified when the contrast was given through a peripheral cannula in the left arm, during subsequent presentation of stroke [20].
Echocardiograms, however, provide evidence of abnormal drainage only. In order to delineate the course of the anomalous vessel other imaging modalities with contrast such as CT and MRI should be performed. They not only provide better visualization of the thoracic venous system and its drainage pattern, but also give accurate anatomical details about the presence of various associated cardiac defects [19].
The literature on treatment options for PLSVC is scarce and the indications for treatment are not well defined. Most of the proposed management options are invasive, including percutaneous occlusion of the PLSVC and surgical re-routing of the PLSVC to the right heart circulation. These procedures are mainly performed when there are clinical complications from venous-to-systemic shunt [9,21]. Although major guidelines do not stipulate usage of anti-coagulation in this clinical context, our patient was started on a NOAC to combat the ongoing risk of CVAs from paradoxical embolization via the PLSVC. This was effective in our patient at preventing further embolic events. It is a novel strategy that can be considered in patients presenting with paradoxical emboli secondary to a PLSVC that are either considered unsuitable for percutaneous intervention or refuse it.
Conclusion
In a setting of a cryptogenic CVA, it is important to consider the presence of PLSVC causing paradoxical embolization as a missed diagnosis of this condition can result in a missed opportunity to provide treatment and prevent further strokes. Echocardiography and TOE are useful investigation modalities in making the diagnosis. Bubble contrast study injected from the left and right arms should be carried when performing an echocardiogram to assess possible anomalous thoracic venous drainage and intra-cardiac shunts.
Disclosure
The authors have no relationships with the industry, financial associations or conflicts of interest to disclose.
References
01. Lanz J, Brophy JM, Therrien J, Kaouache M, Guo L, et al. Stroke in adults with congenital heart disease: Incidence, cumulative risk, and predictors. Circulation. 132(25): 2385-2394 (2015).
02. Windecker S, Stortecky S, Meier B. Paradoxical embolism. J Am Coll Cardiol. 64(4): 403-415 (2014).
03. Yousaf M, Malak SF. Left atrial drainage of a persistent left superior vena cava. J Radiol Case Rep. 3(4): 225 (2008).
04. Zhou Q, Murthy S, Pattison A, Werder G. Central venous access through a persistent left superior vena cava: A case series. J Vasc Access. 17(5): 143-147 (2016).
05. Bulsara SS, Paliwal V, Prasad G, et al. Vascular access in a rare case of ‘isolated-persistent left superior vena cava’. J Vasc Access. 19(4): 409-410 (2018).
06. Tsang W, Boulos M, Moody AR, Sahlas DJ, Morgan CD. An unusual cause of stroke-the importance of saline contrast echocardiography. Echocardiography. 25(8): 908-910 (2008).
07. Ratliff HL, Yousufuddin M, Lieving WR, Watson BE, Malas A, et al. Persistent left superior vena cava: Case reports and clinical implications. Int J Cardiol. 113(2): 242-246 (2006).
08. Bisoyi S, Jagannathan U, Dash AK, Tripathy S, Mohapatra R, et al. Isolated persistent left superior vena cava: A case report and its clinical implications. Ann Card Anaesth. 20: 104-107 (2017).
09. Tobbia P, Norris LA, Lane T. Persistent left superior vena cava draining into the left atrium. BMJ Case Rep. (2013).
10. Rossi UG, Rigamonti P, Torcia P, Mauri G, Brunini F, et al. Congenital anomalies of superior vena cava and their implications in central venous catheterization. J Vasc Access. 16(4): 265-268 (2015).
11. Goyal SK, Punnam SR, Verma G, Ruberg FL. Persistent left superior vena cava: A case report and review of literature. Cardiovasc Ultrasound. 6: 1-4 (2008).
12. Balasubramanian S, Gupta S, Nicholls M, Laboi P. Rare complication of a dialysis catheter insertion. Clin Kidney J. 7(2): 194-196 (2014).
13. Kute VB, Vanikar AV, Gumber MR, Shah PR, Goplani KR, et al. Hemodialysis through persistent left superior vena cava. Indian J Crit Care Med. 15(1): 40-42 (2011).
14. Horlitz M, Schley P, Thiel A, Shin D-I, Müller M, et al. Wolff-Parkinson-White syndrome associated with persistent left superior vena cava. Clin Res Cardiol. 95(3): 133-135 (2006).
15. Hsu LF, Jaïs P, Keane D, et al. Atrial fibrillation originating from persistent left superior vena cava. Circulation. 109(7): 828-832 (2004).
16. Schummer W, Schummer C, Fröber R. Persistent left superior vena cava and central venous catheter position: clinical impact illustrated by four cases. Surg Radiol Anat. 25(3-4): 315-321 (2003).
17. Ebink C, Bos LJ, Vonken EP, et al. An unusual presentation with persistent left superior vena cava. Neth Heart J. 12(2): 69-71 (2004).
18. Recto MR, Sadlo H, Sobczyk WL. Rare case of persistent left superior vena cava to left upper pulmonary vein: pathway for paradoxical embolization and development of transient ischemic attack and subsequent occlusion with an amplatzer vascular plug. J Invasive Cardiol. 19(10): E313-E316 (2007).
19. Lee MS, Pande RL, Rao B, Landzberg MJ, Kwong RY. Cerebral abscess due to persistent left superior vena cava draining into the left atrium. Circulation. 124(21): 2362-2364 (2011).
20. Park CJ, Upadhya B, Pu M, Zhou L. Diagnosis of persistent left superior vena cava: Lessons learned from a recurrent stroke case. Case (Phila). 4(5): 320-323 (2020).
21. Troost E, Gewillig M, Budts W. Percutaneous closure of a persistent left superior vena cava connected to the left atrium. Int J Cardiol. 106(3): 365-366 (2006).